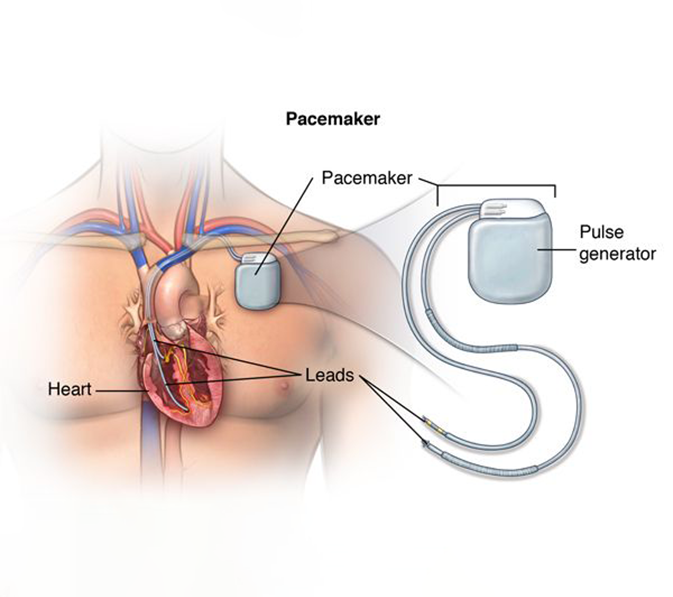
A pacemaker is a small device that&#s placed (implanted) in the chest to help control the heartbeat It&#s used to prevent the heart from beating too slowly Implanting a pacemaker in the chest requires a surgical procedure
A pacemaker is also called a cardiac pacing device
Types
Depending on your condition, you might have one of the following types of pacemakers
- Single chamber pacemaker This type usually carries electrical impulses to the right ventricle of your heart
- Dual chamber pacemaker This type carries electrical impulses to the right ventricle and the right atrium of your heart to help control the timing of contractions between the two chambers
- Biventricular pacemaker Biventricular pacing, also called cardiac resynchronization therapy, is for people who have heart failure and heartbeat problems This type of pacemaker stimulates both of the lower heart chambers (the right and left ventricles) to make the heart beat more efficiently
-
Pacemakers work only when needed If your heartbeat is too slow (bradycardia), the pacemaker sends electrical signals to your heart to correct the beat
Some newer pacemakers also have sensors that detect body motion or breathing rate and signal the devices to increase heart rate during exercise, as needed
A pacemaker has two parts:
- Pulse generator This small metal container houses a battery and the electrical circuitry that controls the rate of electrical pulses sent to the heart
- Leads (electrodes) One to three flexible, insulated wires are each placed in one or more chambers of the heart and deliver the electrical pulses to adjust the heart rate However, some newer pacemakers don&#t require leads These devices, called leadless pacemakers, are implanted directly into the heart muscle
- Risks
Complications related to pacemaker surgery or having a pacemaker are uncommon, but could include:
- Infection near the site in the heart where the device is implanted
- Swelling, bruising or bleeding at the pacemaker site, especially if you take blood thinners
- Blood clots (thromboembolism) near the pacemaker site
- Damage to blood vessels or nerves near the pacemaker
- Collapsed lung (pneumothorax)
- Blood in the space between the lung and chest wall (hemothorax)
- Movement (shifting) of the device or leads, which could lead to cardiac perforation (rare)
-
Before your doctor decides if you need a pacemaker, you&#ll have several tests done to find the cause of your irregular heartbeat Tests done before you get a pacemaker could include:
- Electrocardiogram (ECG or EKG) This quick and painless test measures the electrical activity of the heart Sticky patches (electrodes) are placed on the chest and sometimes the arms and legs Wires connect the electrodes to a computer, which displays the test results An ECG can show if the heart is beating too fast, too slow or not at all
- Holter monitoring A Holter monitor is a small, wearable device that keeps track of the heart&#s rhythm Your doctor may want you to wear a Holter monitor for to days During that time, the device records all of your heartbeats Holter monitoring is especially useful in diagnosing heartbeat problems that occur at unpredictable times Some personal devices, such as smartwatches, offer electrocardiogram monitoring Ask your doctor if this is an option for you
- Echocardiogram This noninvasive test uses sound waves to produce images of the heart&#s size, structure and motion
- Stress test Some heart problems occur only during exercise For a stress test, an electrocardiogram is taken before and immediately after walking on a treadmill or riding a stationary bike Sometimes, a stress test is done along with echocardiography or nuclear imaging
- Before the procedure
You&#ll likely be awake during the surgery to implant the pacemaker, which typically takes a few hours A specialist will insert an IV into your forearm or hand and give you a medication called a sedative to help you relax Your chest is cleaned with special soap
Most pacemaker implantations are done using local anesthesia to numb the area of the incisions However, the amount of sedation needed for the procedure depends on your specific health conditions You may be fully awake or lightly sedated, or you may be given general anesthesia (fully asleep)
During the procedureOne or more wires are inserted into a major vein under or near your collarbone and guided to your heart using X-ray images One end of each wire is secured at the appropriate position in your heart, while the other end is attached to the pulse generator, which is usually implanted under the skin beneath your collarbone
A leadless pacemaker is smaller and typically requires a less invasive surgery to implant the device The pulse generator and other pacemaker parts are contained in a single capsule The doctor inserts a flexible sheath (catheter) in a vein in the groin and then guides the single component pacemaker through the catheter to the proper position in the heart
After the procedureYou&#ll likely stay in the hospital for a day after having a pacemaker implanted Your pacemaker will be programmed to fit your heart rhythm needs You&#ll need to arrange to have someone drive you home from the hospital
Your doctor might recommend that you avoid vigorous exercise or heavy lifting for about a month Avoid putting pressure on the area where the pacemaker was implanted If you have pain in that area, ask your doctor about taking medicines available without a prescription, such as acetaminophen (Tylenol, others) or ibuprofen (Advil, Motrin IB, others)
Special precautionsIt&#s unlikely that your pacemaker would stop working properly because of electrical interference Still, you&#ll need to take a few precautions:
- Cellphones It&#s safe to talk on a cellphone, but keep your cellphone at least inches ( centimeters) away from your pacemaker Don&#t keep your phone in a shirt pocket When talking on your phone, hold it to the ear opposite the side where your pacemaker was implanted
-
Security systems Passing through an airport metal detector won&#t interfere with your pacemaker, although the metal in the pacemaker could sound the alarm But avoid lingering near or leaning against a metal-detection system
To avoid potential problems, carry an ID card stating that you have a pacemaker
- Medical equipment Make sure all your doctors and dentists know you have a pacemaker Certain medical procedures, such as magnetic resonance imaging, CT scans, cancer radiation treatment, electrocautery to control bleeding during surgery, and shock wave lithotripsy to break up large kidney stones or gallstones could interfere with your pacemaker
- Power-generating equipment Stand at least feet ( centimeters) from welding equipment, high-voltage transformers or motor-generator systems If you work around such equipment, ask your doctor about arranging a test in your workplace to determine whether the equipment affects your pacemaker
-
Devices that are unlikely to interfere with your pacemaker include microwave ovens, televisions and remote controls, radios, toasters, electric blankets, electric shavers, and electric drills
ResultsHaving a pacemaker should improve symptoms caused by a slow heartbeat such as fatigue, lightheadedness and fainting Because most of today&#s pacemakers automatically adjust the heart rate to match the level of physical activity, they may can allow you to resume a more active lifestyle
Your doctor should check your pacemaker every to months Tell your doctor if you gain weight, if your legs or ankles get puffy, or if you faint or get dizzy
Most pacemakers can be checked by your doctor remotely, which means you don&#t have to go into the doctor&#s office Your pacemaker sends information to your doctor, including your heart rate and rhythm, how your pacemaker is working, and how much battery life is left
Your pacemaker&#s battery should last to years When the battery stops working, you&#ll need surgery to replace it The procedure to change your pacemaker&#s battery is often quicker and requires less recovery time than the procedure to implant your pacemaker
Pacemakers and end-of-life issuesIf you have a pacemaker and become terminally ill with a condition unrelated to your heart, such as cancer, it&#s possible that your pacemaker could prolong your life Doctors and researchers vary in their opinions about turning off a pacemaker in end-of-life situations
Talk to your doctor if you have a pacemaker and are concerned about turning it off You may also want to talk to family members or another person designated to make medical decisions for you about what you&#d like to do in end-of-life care situations
